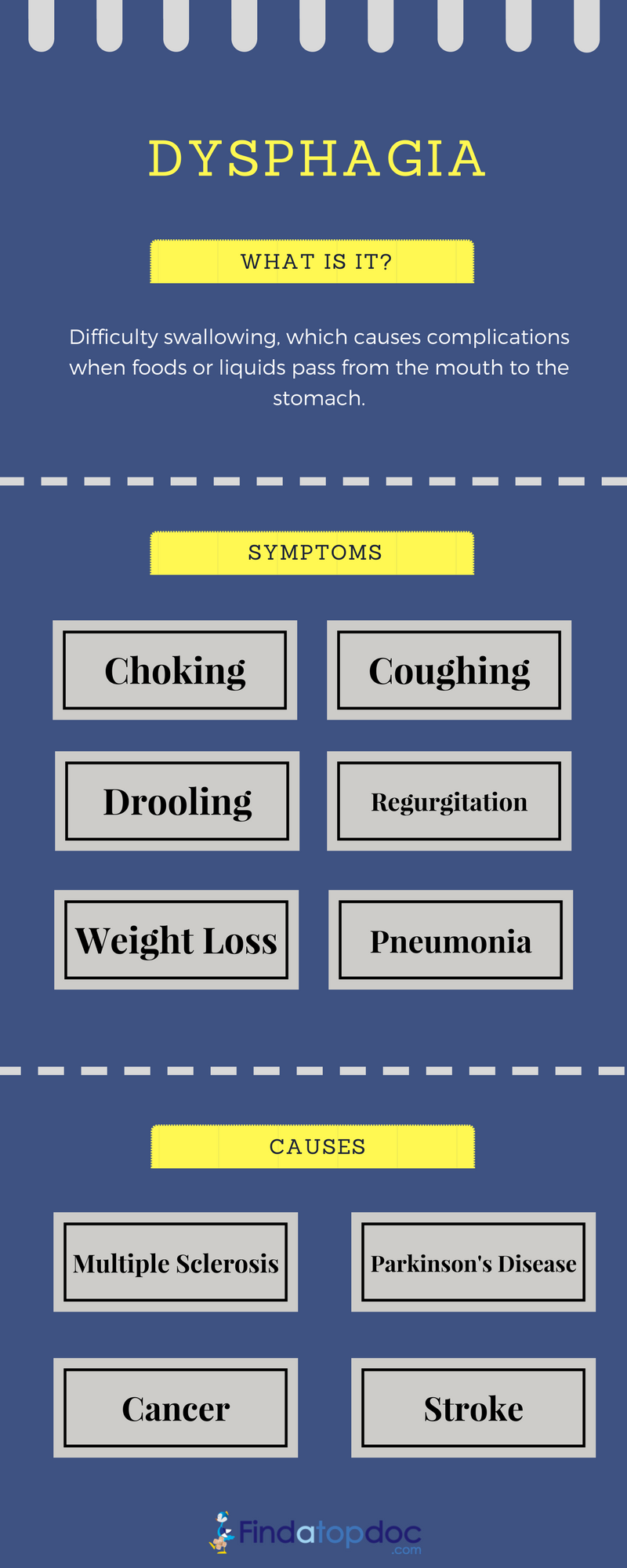
The disease dysphagia mainly concerns difficulty swallowing, which causes trouble when passing food from the mouth to the stomach. The disease occurs due to nerve or muscle problems, which become more common among older people. Although the medical term "dysphagia" is often regarded as a symptom of something else, it is sometimes a condition in its own right.
Dysphagia is difficulty swallowing and can be caused by a number of factors, including muscle and nerve problems.
The chewing process involves seeing, smelling, and tasting. It allows you to smell or taste food or drink, which produces saliva that is designed to make chewing easier. When you chew food, it becomes a soft bolus (a mass of food that is ready to swallow). The tongue pushes the bolus to the back of the mouth to the pharynx. From this moment onward, the swallowing movement is a reflex action, meaning it is automatic. The larynx, or voice box, closes and prevents food and liquid from going down the windpipe into the lungs. The gulping action pushes the food into the esophagus, which has muscular walls that move the food down to the stomach.
Dysphagia is mainly caused by the swallowing process described above. There are two main types of dysphagia; one is oropharyngeal dysphagia, or high dysphagia, which mainly affects the mouth and/or throat and is caused by tongue weakness after having a stroke, or difficulties making saliva. Issues in the throat are often caused by a neurological problem that affects the nerves and can cause Parkinson's disease, stroke, or amyotrophic lateral sclerosis.
The other type of dysphagia is esophageal dysphagia, or low dysphagia, which affects the esophagus. This is usually due to a blockage or irritation. Often, a surgical procedure is required.
It is worth noting that pain when swallowing (odynophagia) is different from dysphagia, but it is possible to have both at the same time.
Globus is the sensation of something being stuck in the throat without dysphagia.
Patients may have dysphagia and be unaware of it. In some cases, the disease goes undiagnosed and is not treated until it becomes serious. It can raise the risk of aspiration pneumonia, which is mainly a lung infection that can develop when you inhale saliva or food particles. The aspiration means inhaling the food into the lungs, or swallowing the food without biting or chewing.
Symptoms of dysphagia include:
- Choking while eating
- Cough while swallowing
- Drooling food
- Stomach acid backing up into the throat
- Getting regular heartburn
- Rough voice
- Food getting stuck in the throat or chest
- Food getting stuck behind the breastbone
- Sudden weight loss
- Regurgitation
- Difficulty holding food in the mouth
- Difficulty swallowing (i.e., gulping)
- Persistent pneumonia
- Inability to hold saliva in the mouth
- Getting food stuck in the mouth
Treatment for dysphagia depends on the type or cause of dysphagia.
Oropharyngeal dysphagia
Therapy may include:
- Certain exercises may help to improve the coordinating of swallowing muscles or restimulate the nerves that trigger the swallowing reflex.
- Learning swallowing techniques, such as ways to place food in the mouth or how to position the body and head when swallowing .
Esophageal dysphagia
Treatment approaches for esophageal dysphagia may include:
- Esophageal dilation. Doctors may use an endoscope with a special balloon for a tight esophageal sphincter (achalasia) or an esophageal stricture. This balloon is attached gently stretch and expand the width of the esophagus.A flexible tube may also be used to dilate the esophagus. Surgery is usually recommended for patients with an esophageal tumor, achalasia or pharyngeal diverticula. This helps to clear your esophageal path.
- Difficulty swallowing associated with GERD can be treated with prescription oral medications to reduce stomach acid.
- Patients with eosinophilic esophagitis may need corticosteroids. If a patient has esophageal spasm but the esophagus appears normal and without GERD, he or she may be treated with medications to relax the esophagus and reduce discomfort.
If dysphagia prevents a patient from eating and drinking adequately, a doctor may recommend special liquid diet to help the patient maintain a healthy weight and avoid dehydration. A feeding tube is required in severe cases of dysphagia.
Dysphagia can't be prevented. However, the risk of occasional difficulty swallowing can be reduced by eating slowly and chewing food well.
Early detection and effective treatment of GERD can lower the risk of developing dysphagia associated with an esophageal stricture.
Lifestyle modifications are necessary in order to cope with dysphagia.
The following tips can help to relieve some symptoms of dysphagia:
- Changing eating habits by eating smaller, more frequent meals.
- Cutting food into smaller pieces and eating more slowly. Trying foods with different textures to see if some cause more trouble when swallowing.
- Thin liquids, such as coffee and juice, are a problem for some people, and sticky foods, such as peanut butter or caramel, can make swallowing difficult.
- Avoiding foods that cause trouble. Avoiding alcohol, tobacco, and caffeine as these can make heartburn worse.
Other recommendations include:
-
Swallowing therapy: This involves exercises to control tongue movement and others for speech and language.
-
Diet: in this therapy, the patients are made aware of nutritious food items and the food and liquid products that are easy to swallow.
-
Balanced diet: Feeding through a tube is useful for patients who are at risk of pneumonia.
These therapies are highly useful and allow a person suffering from swallowing difficulties to overcome the issues.