What Causes Lupus?

Lupus is an autoimmune ailment. This means that instead of your body’s regular defense system attacking viruses and bacteria, it destroys healthy tissues. This causes swelling. Symptoms include extreme fatigue, hair loss, rashes, cognitive dysfunction, severe muscle and joint pain, ulcers in the mouth or nose. If lupus is not treated, then it can cause organs damage and failure. It can be potentially fatal.
A number of people with lupus only have mild symptoms. The disease can be survived but you have to learn to live with it. To prevent too much injury to their organs, most people usually control the warning signs. You can prevent damage to your organs through regular checkups with the doctor, rest, workouts, and the proper medications.
Types of lupus
They are of four types
- Discoid lupus erythematosus- it usually affects the skin hence known as cutaneous lupus.
- Drug induced lupus erythematosus- it may occur due to side effect of certain drugs which are used to treat certain conditions. For example, beta blockers used to treat heart disease and hypertension.
- Neonatal lupus erythematosus- it is found in newborn babies whose mother have the disease and is of the rare type. It can cause complication of birth or may cause a severe heart defect.
- Systemic lupus erythematosus- this causes multiple organs and systems of the body to get inflamed.
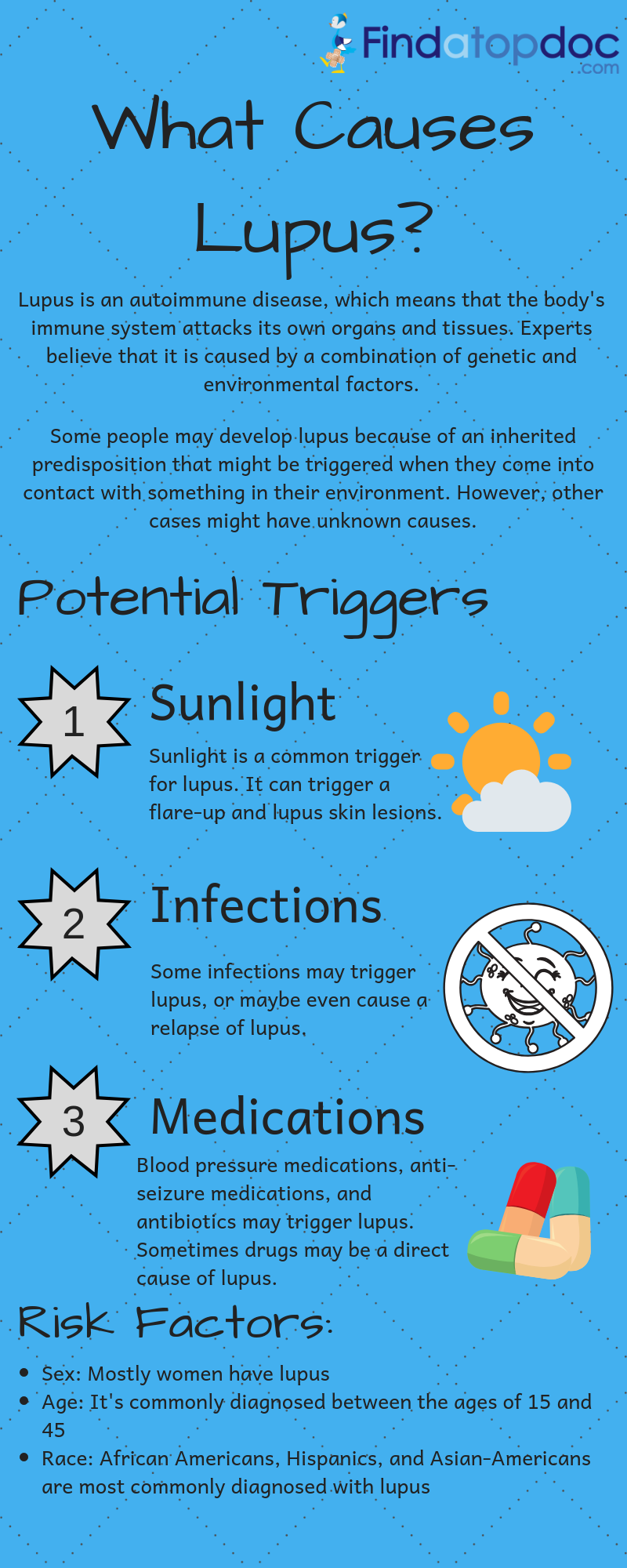
What causes lupus?
This is a difficult question to answer. Research has not clearly confirmed what really causes lupus. Luckily, lupus is not contagious, though there are several elements that can help determine a person’s chances of developing lupus.
No one knows the real cause of lupus. Experts however do believe that there are certain genes that determine how the whole immune system works in some people. Apart from that, there are numerous factors that activate a lupus attack. Examples are viral infection and sunlight.
People with lupus are affected differently by different triggers. Most scientists, however, believe that a combination of several factors both inside and outside the body cause lupus to develop. These factors include hormones, genetics, and environment.
Causes of lupus
- Hormones
Hormones are chemical substances. They control and regulate the activity of certain cells. Most of the body’s functions are regulated by the hormones; the body uses these hormones as messengers. Researchers are working round the clock to establish the relationship between lupus and estrogen because statistics show that nine out of ten incidences of lupus occur in women.
Both men and women produce estrogen but women produce much more. Estrogen is believed to be an “immunoenhancing hormone”. It means that immune system of women is much stronger than that of men. Hence the autoimmune diseases are generally higher in men than in women. Studies also show that many women show lupus symptoms before a menstrual period and/or when they are expecting a baby, both instances during which estrogen production is very high.
This may indicate that lupus is in some way correlated with estrogen. There has not been any proof, however, of the connection between estrogen or any other hormone and lupus. Neither have studies shown any increase in the activity of the illness when women are taking birth control pills or during postmenopausal therapy.
- Genetics
So far, no gene or group of genes have been associated to cause lupus. Certain genes however have been recognized and can give an understanding into a person’s chances of getting lupus. Patients with symptoms of lupus are usually asked if one of their family member has lupus. The occurrence of lupus in certain ethnicity and clustering of lupus in families drew researchers to make a connection between genes and lupus.
For example, couples with lupus have a risk of a child developing lupus 20 times more than the overall population. Moreover, family members of people with lupus who are otherwise healthy might come out positive in several lupus-related medical tests. But it doesn’t mean the gene’s presence predisposing the person to lupus will always develop the disease. People with no family history of lupus can also develop the condition.
There are 2 families of genes, represented as major histocompatibility complex class (MHC) II and III, identified to be linked with lupus. The MHC gene assists in improving your immune reaction by coding for proteins the way they should respond to invaders. When the MHC II gene and lupus come together, their strength varies by ethnicity. The complement system on the other hand is assisted by the MHC II gene to code for components, a collection of proteins that comes together to get rid of immune complexes and upset the body’s inflammatory reaction. Lupus includes flaws of the genes for supplement proteins C4 and C2.
Other genes too are linked with lupus development. Among them are genes which code for different forms of opsonins, molecules which help cells in the protective response to proceed with certain steps. Opsonins are precisely involved with assisting in phagocytosis, a process whereby cells known as macrophages gulp antibodies carrying attacking particles. The opsonins that carry this are proteins known as mannose binding protein as well as C-reactive protein.
Also known to be associated with lupus are genes that code for antibody receptors and complement receptors. These receptors are responsible for finding and linking to pathogens in the body. Also linked with lupus are cytokines genes, molecules that work as gesturing molecules in your protected system. Tumor necrosis factor-α (TNF-α) as well as interleukin-10 (IL-10) are cytokines that researchers are focusing on in detail.
Fcy-receptors gene which code for the molecules whose work is to get hold of antibodies that are carrying antigens has been linked with lupus nephritis. This is lupus that affects the kidneys. Researchers are looking in detail for different forms of this gene which make these receptors work poorly, triggering the inefficient removal of protected system cells from the body.
A group of genes on chromosome 6 codes for HLA (human leukocyte antigens). These antigens play an important role in making person susceptible and resistant to disease. Development of many common disorders may be influenced by specific HLA antigens. If a person has the specific HLA antigen type associated with this disease, then they may be genetically more susceptible to have this condition and may have more chances of developing it. The antigens associated with lupus are DR2 and DR3. However, person without these antigens too may develop the disease. Hence these specific HLA antigens cannot be used for diagnostic testing or cannot give an accurate prediction of the disease.
However, no specific gene or group of gene has been known or been proven to cause lupus. Certain genes that contribute to the development of lupus have been identified. It is more common among some families. Genetic associations alone are not conclusive for causing lupus. It can be highlighted in the following case wherein only one of the twins develops the disease. Identical twins may have brought up in the same environment and may share the same inherited attributes. But any one of them may develop the disease.
The chances of identical twin developing the disease are 25% and for fraternal twins it is 2-3%. On sibling of individuals with the disease, the risk of developing lupus is 20 times higher than the general population. Lupus may also develop in people who do not have any family history of the disease. But there may be cases of other autoimmune diseases in some family members such as thyroiditis, hemolytic anemia, idiopathic thrombocytopenia purpura.
People of ethnic groups such as African, Asian, native American, native Hawaiian, Hispanic, or Pacific Island descent have a higher risk of developing the disease than Caucasians. Caucasian may show mild manifestation of lupus. The survival rate of Caucasians after five years was around 94-96 percent whereas African, Asian ethnicities with lupus had survival rate is close to 79-92 percent. The common cause of death in Caucasian with lupus was complication involving the cardiovascular system, respiratory problems and malignancy problems.
Lupus is most common in ages between 15 to 44 although it may develop at any age. The disease manifestations are more acute in the younger age. The one with juvenile onset lupus are more vulnerable to the mucocutaneuous manifestations such as alopecia, skin rash or ulcers in the mucous membrane. However, the mortality rate is much higher in patients with late onset lupus. Half of them die of their affliction.
Biomarkers
This is another significant area of research which is associated with lupus. Biomarkers are molecules. They reflect specific or particular biological or pathological process, a response to therapeutic intervention, a consequence of a process. Biomarkers allow the doctor to know what is happening in the body of a person or help predict what is going to happen. The following have been identified as potential biomarkers by researchers.
- Anti double stranded DNA antibodies and complement C3a1 both can be shown in blood tests as biomarkers for flares.
- C-reactive protein-it is a protein made by the liver. It helps correlate the activity of the diseases and the risk factors of cardiovascular diseases and C4d.
C4d is a protein that is found in the blood and it indicates the activity of lupus disease or involvement of the kidney.
Another biomarker is presence of protein in the urine of people with renal disease which is caused by lupus. They help identify the type of disease and the severity of renal disease as well as help to know the extent to which the kidney is damaged.
- Illness
Once people are affected by bacteria and viruses such as parvovirus, epstein-barr, or hepatitis c, they might develop lupus, although there is no direct causal connection that has been established.
- Medication
Some drugs are alleged to set off lupus and warning signs flare up thereby becoming suspected causes of the ailment.
Drug-induced lupus is grounded on this theory. Often, when a patient with medication-induced lupus discontinues using the drugs that are thought to be encouraging the lupus, the warning signs can drop fast and even go away.
- A combination of factors
Many people in the research and medical fields strongly agree that the more factors listed above are present, the more people become susceptible to contracting the disease.
- Environment
Many researchers consider environmental agents like viruses or perhaps a chemical exchange with a genetically-susceptible person acts to initiate the ailment. No specific environmental agent has been confirmed to cause lupus but the assumption remains likely. The environmental factors that cause flares haven’t been identified yet, but ultraviolet light contamination (with the effects of the Epstein-Barr virus included) and exposure to silica dust in agricultural and industrial surroundings have been mentioned.
Other environmental triggers include:
- The sun's ultraviolet rays
- Fluorescent light bulbs' ultraviolet rays
- Drugs that make a person more sensitive to the sun, i.e., Bactrim® and Septra® (trimethoprim-sulfamethoxazole); sulfisoxazole (Gantrisin®); tolbutamide (Orinase®); sulfasalazine (Azulfidine®); diuretics
- Sun-sensitizing tetracycline drugs such as minocycline (Minocin®)
- Other antibiotic drugs or penicillin, i.e., amoxicillin (Amoxil®); ampicillin (Ampicillin Sodium ADD-Vantage®); cloxacillin (Cloxapen®)
- Infection
- Viral illness or cold
- Fatigue
- Wound
- Emotional stress, i.e., divorce, illness, losing a loved one etc.
- Stress caused to the body, i.e., operation, physical harm, pregnancy or child birth.
- Exposure to silica drugs in agricultural or industrial settings.
- Exhaustion
- smoking
Apparently unrelated issues can also cause the development of lupus in a vulnerable person. Some common features noted by scientists include:
- Sun exposure- sunlight exposure may tend to bring on the skin lesions. It may also trigger an internal response in people who are susceptible to this disease.
- Infections- infections can initiate lupus. In some people it may also cause a relapse
- Contamination
- Pregnancy
- Childbirth
- Medication prescribed to treat an illness- certain types of anti-seizure medications, antibiotic and blood pressure medications may trigger lupus. Such people with drug induced lupus observe that once the medications are stopped the symptoms go away
Immune system in lupus
In lupus, the normal immune system does not function properly and the normal mechanism for removing the waste of the cells fails. The immune system of a healthy body protects the body against foreign invaders such as viruses, toxins and bacteria. They mount immune repsonse agaisnt these invaders. The immune response can come in the form of immune cells and protein antibodies. The two typos of immune cells are T cells which are suppressor cells and B cells which are the worker’s cells. B cells produce antibodies. In lupus the suppressor response is impaired and the B cells go into and overdrive and hence produce excess antibodies. These excess antibodies damage the important body parts such as the blood cells and blood vessels.
It has also been found that immune system in a normal healthy body not only neutralizes the invaders but also removes the dead or damaged cells. In lupus the failures of this function leads to a build up of unwanted materials which can be potentially dangerous.
Immunosuppressive are capable of damaging healthy cells hence in future drugs should be given which specifically pinpoint certain cells. One such showing great promise is rituximab (Mabthera). This drug targets a specific marker CD20 on B cell and also has a great effect on antibody –producing cells.
Some causes of systemic lupus
Liquid chlorophyll – this is a cause of systemic lupus. It causes flares in patients with the disease. Liquid chlorophyll made form alfalfa should be avoided by those who have lupus.
Chemical exposure- exposure to chemicals causes lupus but once the chemicals have gone away the disease too goes away, particularly chemicals trichloroethylene in well water and silica dust may increase the risk.
Vitamin D deficiency- people with lupus have less vitamin D in their body. People with lupus tend to avoid sun. One case study has found the possible relation between these two and suggested that this should be used as a biomarker to find the status and the activity of the disease.
Viruses and bacteria- these are considered as potential causes of lupus. Viruses such as cytomegalovirus, hepatitis C, and parvovirus are potential causes.
Chronic unintentional dehydration- lupus can also be caused by not drinking adequate amount of water and unprocessed sea salt in our diet.
At present there is no cure for lupus but effective treatment can be done and majority of the people with the disease can lead a healthy life.
How clinical research trials can help stop causes of lupus
Researchers have learned a lot while trying to find out the causes of lupus. New medications and treatments have been revealed and are now being tested in clinical trials. Even though researchers have not fully understood the causes of lupus, proper care and treatment should be kept to standard. Fighting with a chronic disease whose cause has not yet been figured out can leave you very frustrated and helpless.
Participating in clinical trials is one way of feeling effective and gaining some control.
Benefits of participating in clinical trials are:
Patients are more involved in their own health care.
Gaining the right to use new cures before they are available everywhere.
Assisting others by backing medical research through taking part in clinical trials.
Lupus remains a mysterious disease that doctors are still researching on. But until the causes are discovered, we will continue controlling the symptoms through traditional and alternative treatments as well as trial medications.