What is Lupus?

Lupus is an inflammatory chronic disease that develops when the body immune system attacks and damages its own organs and tissues. Inflammation as a result of lupus can damage different body systems such as the blood cells, brain, joints, skin, lungs, heart and kidneys.
The normal and main function of your immune system is to protect the body by fighting germs, fungi, bacteria, and viruses through production of certain proteins known as antibodies. Antibodies are produced by the lymphocytes. With lupus, the immune system functions differently and cannot tell the difference between foreign invaders and healthy tissues. Antibodies are produced against healthy body tissues, cells, and organs, causing damage, pain and inflammation in different body parts.
Is lupus contagious?
Lupus is not a contagious disease. It is rather a disease of remissions and flare-ups. Its symptoms can range from mild to severe.
The major types of lupus include discoid, drug-induced, and neonatal. Systemic lupus erythematosus is the most severe form of the types, as it affects the major organs in the body including the lungs, kidneys, and the heart. It also attacks the blood. The disease often exists in a pattern with an active period, with prominent symptoms, followed by a remission period during which the disease remains dormant.
The actual cause of the disease is unknown. It is believed that the risk of the disease increases with a combination of genetic and environmental factors. The disease seems to be passed on through generations, as the disease is known to occur in families. Lupus is more common in females than in males, and it is possible that the right genetic condition, when present, is triggered by certain hormones. Environmental factors that are known to trigger the condition include stress, smoking, certain medications, certain infections, exposure to chemicals, and UV light.
Symptoms of lupus appear differently in different people. In some cases, the symptoms appear suddenly, while in others, it may develop gradually. The symptoms may range from mild to severe and they may be temporary, or remain for a long period. The most common symptoms of this disease are pain and swelling in the joints.
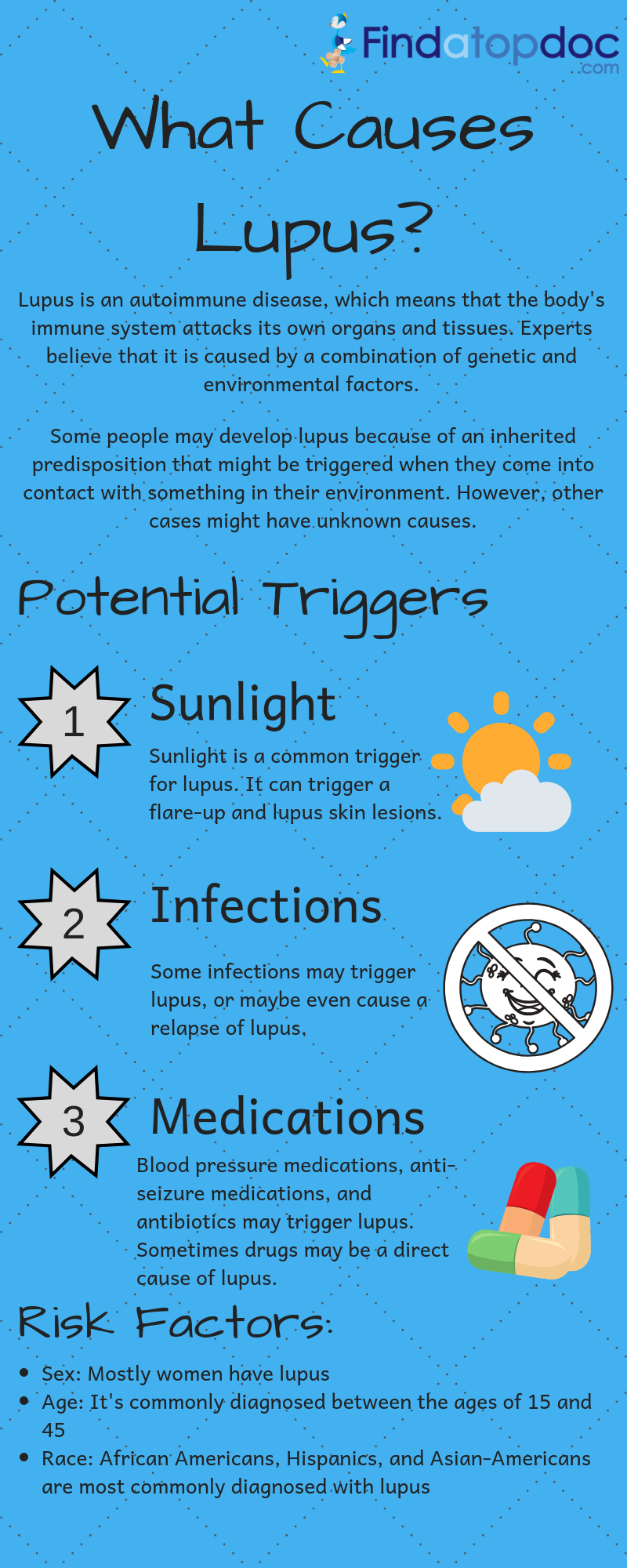
What causes lupus?
How do you get lupus? The exact cause of lupus is not known, but some scientific experts indicate that the cause of lupus is a combination of many factors that are in and out of the body.
Hormones
Hormones are chemical substances produced in the body to regulate and take control of cells' and organs' activities. 90% of lupus cases have been reported in women, suggesting that lupus has a relationship with the estrogen hormone. Though men produce estrogen, women produce more of it, and have a stronger immune systems compared to men.
For this reason, women are more prone to autoimmune diseases compared to men. Flare-ups of lupus symptoms in women increase during menstrual periods and pregnancy when there are high levels of estrogen. This may suggest that estrogen controls the severity of lupus signs and symptoms.
Genetics
Is lupus hereditary? The disease may be hereditary.
Though no gene or group of genes have been seen to cause lupus, some families are more prevalent to it, meaning that some genes are contributing to its development.
Lupus may develop in people with no family history of the disease, but there is likelihood of a history of other autoimmune diseases such as hemolytic anemia and thyroiditis.
Biomarkers
Biomarkers are molecules that help reflect a specific pathological or biological process, the effect of the process, and its response to medications. Biomarkers can simply help your doctor understand what is happening in your body and predict what is likely to happen based on the normality of the cells, tissues and body fluids.
Some potential biomarkers that may indicative of lupus include:
- C-reactive protein, a protein in the liver that correlates with lupus
- Anti-double-stranded DNA antibodies
- Proteins in the urine for people with nephritis
- Complement C3a
Environment
The following environmental factors are believed to be risk factors for lupus in genetically susceptible individuals:
- Smoking
- UV rays from the sun and fluorescent light bulbs
- Sulfa drugs such as diuretics
- Injury
- Exhaustion
- Viral colds
- Antibiotics such as penicillin, ampicillin and amoxicillin
- Exposure to silica
- Tetracycline drugs
- Infections such as Epstein Barr virus infection
- Emotional stress
Types of lupus
Lupus is a condition that exists in different forms as discussed below.
Discoid Lupus Erythematosus (DLE)
DLE is a type of lupus that is characterized by a chronic skin disorder, with raised and red rashes that appear on the face, scalp, or any other body part.
In DLE, the raised rash becomes thick and forms scars. The rash on the skin can last for several days before it goes away.
Systemic Lupus Erythematosus (SLE)
SLE is the most common type of lupus. "Systemic" means that the condition can affect almost all parts of the body.
The symptoms of SLE can range from mild to severe. Severe symptoms of SLE mainly occur in people aged 15 to 45 years. SLE can develop during childhood or at old age.
Subacute cutaneous lupus erythematosus
Subacute cutaneous lupus erythematosus is a type of lupus characterized by multiple skin lesions appearing on different parts of the body that are exposed to direct sunlight. Lesions in this type of lupus do not form scars.
Drug induced lupus
Drug-induced lupus is caused by a number of drugs or medications such as antifungals, high blood pressure medications, antibiotics, anti-seizure medications, and oral contraceptive drugs.
The signs and symptoms of drug-induced lupus typically disappear after you stop taking the drugs.
Neonatal Lupus
This is a rare type of lupus that occurs mainly in infants and women with Systemic Lupus Erythematosus or no disease at all. Contrary to this, many babies of Systemic Lupus Erythematosus mothers are born healthy.
Many scientists believe that neonatal lupus is caused by autoantibodies that are found in the mother’s blood. Such autoantibodies are anti-La (SSB) and anti-Ro (SSA).
During birth, the babies with such type of lupus have low blood counts, skin rash and liver problems. Such symptoms typically disappear after the child reaches 6 months of age.
What are the symptoms of lupus?
Signs and symptoms of lupus may range from mild to severe. The symptoms may also manifest differently in different people.
Such signs and symptoms include:
- Anxiety and loss of memory
- A feeling of tiredness
- Swelling and joint pains
- Rash on the skin
- Delirium or a state of confusion
- Hair loss that is unusual
- Respiratory problems such as chest pain during deep breathing
- Chills and fever
- Swelling around the eyes and on the legs (edema)
- Swollen glands, especially the lymph nodes
Signs of lupus may also manifest in the following body organs:
- Lungs: Lupus can make people develop pleuritis. This is an inflammation of the inner lining of the pleural cavity that can cause pain on the chest mainly when breathing deeply. Pneumonia may also develop in patients with lupus.
- Kidneys: Lupus can also cause kidney nephritis that can impair the ability of the kidney to eliminate waste materials effectively.
- Central nervous system: Lupus can also affect the central nervous system or the brain causing vision problems, memory loss, headaches, seizures, dizziness, depression and stroke.
- Blood: Lupus patients can develop leukopenia (decreased number of leucocytes), anemia and thrombocytopenia (decreased number of platelets).
- Blood vessels: Lupus may cause inflammation of the blood vessels a condition known as vasculitis. This may affect the system of blood flow in the body.
- Heart: Some of the lupus patients can develop inflammation of the heart (endocarditis) or the membrane that surrounds the heart (pericarditis) causing chest pain among other symptoms. Endocarditis can cause damage to the heart valves leading to heart murmurs.
How is lupus diagnosed?
Diagnosis for lupus is a very complicated process.
To make a correct diagnosis for lupus, the doctor and patient need to work together. Typically, a lupus diagnosis is done through process of elimination. An accurate medical history from the patient, physical examination and laboratory tests can help the doctor know whether you have lupus or not.
The most important tests that help in diagnosis identify some autoantibodies that are present in a lupus patient’s blood. An antinuclear antibody (ANA) is an example of a test used to look at antibodies that may react against the nucleus components of body cells.
Some of the tools used in diagnosis of lupus include:
- Biopsy of the skin
- Medical history of the patient
- Laboratory tests that may include complete blood count (CBC), blood chemistry, erythrocyte sedimentation rate (ESR), ANA, immune complement levels, and other autoantibody tests
- Physical examination
- Biopsy of the kidney
Blood tests
In diagnosis for lupus, patients who are found to have positive ANA need more tests to check for any other antibodies. Any autoantibodies can give more information about any autoimmune disease present in someone.
To check for other antibodies, blood tests are done which help identify the following 6 antibodies:
- Anti-Smith antibody: This is a ribonucleoprotein that is found in the nucleus of any cell. This protein is present in about 20% of patients with lupus. Anti-SM antibody does not correlate in the case of kidney lupus.
- Antiphospholipid antibodies (APLs): These are directed against phospholipids. They are present in about 60% of lupus patients.
- Anti-double-stranded DNA antibody: This is a type of ANA antibody that is found in about 30% of patients with lupus. Presence of this type of antibody identifies a more severe form of lupus such as kidney lupus (lupus nephritis).
- Anti-Ro and Anti-La antibodies: These are antibodies that are found in about 40% of lupus patients and patients with primary Sjögren's syndrome. The antibodies are mostly found in lupus patients who have tested negative for ANA.
- Anti-UIRNP antibodies: These antibodies are found alongside anti-SM antibodies in patients with lupus. They are found in about 25% lupus patients. These antibodies have been linked with features of scleroderma such as Raynaud’s phenomenon.
- Anti-histone antibodies: These are antibodies that are commonly found in patients with drug-induced lupus and rarely in patents with SLE. However, these antibodies are not that specific enough to lupus conditions and cannot be used to make a concrete diagnosis.
Urine tests
Apart from blood tests, urine tests can also be used to diagnose and monitor all the effects of lupus in the kidneys.
These urine tests include:
- Measurement of proteinuria and glomerular filtration rate: It is a test that is used to measure how effective your kidneys are in filtering waste products. This test is performed on urine that has accumulated in over 24 hours.
- Urinalysis: This is a test that is used to test for any kidney disease. Urinalysis can tell the presence of white blood cells, proteins, red blood cells, and cellular abnormalities in the urine that signal a kidney disease.
- Protein to creatinine ratio: This is a test that is done on a one-time urine sample. It helps your doctor measure any loss of protein that would signal a kidney malfunction.
Serum complement test
This is a test that is used to measure the levels of proteins that are used during the inflammation process. Low complement levels signifies that the inflammation is taking place inside the body.
Complement levels may vary differently in different people due to genetic factors.
Treatment for lupus
If you are diagnosed with lupus , you may need a group of specialists to help treat it.
Such specialists may include:
- Nephrologists: Specialists who treat kidney diseases
- A family doctor: He/she can help in giving your medical history and medical progress
- Dietitians
- Rheumatologists: Doctors who treat arthritis and other joints inflammatory diseases
- Clinical immunologists: Doctors who deal with immune system diseases
- Hematologists: Doctors who treat blood disorders
- Cardiologists: Doctors who treat blood vessel disorders and heart diseases
- Dermatologists: Specialists who treat skin conditions
- Endocrinologists: Doctors who treats any diseases related to hormones and glands
Once you have been diagnosed with lupus, a rheumatologist will develop a lupus treatment plan for you depending on your health, age, sex, lifestyle, and severity of symptoms. Treatment plans can also be developed depending on the patient’s needs.
When developing a treatment plan, your doctor's main goal is to:
- Reduce any organ damage and other body problems
- Prevent flare-ups
- Treat any flare-ups when they occur
Lupus treatment may include medications intended to:
- Boost the immune system
- Balance body hormones
- Reduce pain and swelling
- Reduce or prevent flare-ups
- Prevent or reduce joints damage
Some medications that have been used to treat the symptoms of lupus completely include:
- Hydrxychloroquine: This is an antimalarial drug that has been successfully used to treat mild symptoms of lupus such as joint disease and lupus rash.
- Corticosteroids: Some steroids such as prednisone and steroids creams are drugs that can successfully treat rashes associated with lupus.
- Azathioprine: This is a drug that is mostly used to prevent organ rejection during organ transplantation. It can be used to treat severe symptoms of lupus.
- Methotrexate: This is a chemotherapy medication that is used to suppress the immune system. It can be used to treat some symptoms of lupus such as skin rash and joint pains that do not respond to steroids.
- Cyclophosphamide: This is a chemotherapy medication that is used to suppress the immune system. It can be used to treat severe symptoms and signs of lupus.
- Rituximab: This is a monoclonal antibody that can be used to reduce the activity of the lymphocytes that produce the autoantibodies.
- Belimumab: It is another monoclonal antibody that also helps reduce the lymphocytes' activity. Lymphocytes are cells that make the autoantibodies.
So far, any complementary or alternative therapies such as nutritional supplements, special diets, ointments, fish oils, creams, homeopathy and chiropractic treatments have not been found to cure lupus or prevent organ damage.
However, some complementary approaches have been found to help the patient live with lupus and manage symptoms.
Is lupus fatal?
No, the disease is not universally fatal. With proper treatment and close follow-up, more than 90% of lupus patients live a long and normal life.
However, some severe symptoms of lupus are difficult to treat or manage and may have an impact on daily activities.