Nosebleed is a very common occurrence, particularly in children aged 3-10 years and adults in the age group of 50-80 years. Most forms of nosebleeds are not serious, although it is a scary symptom.
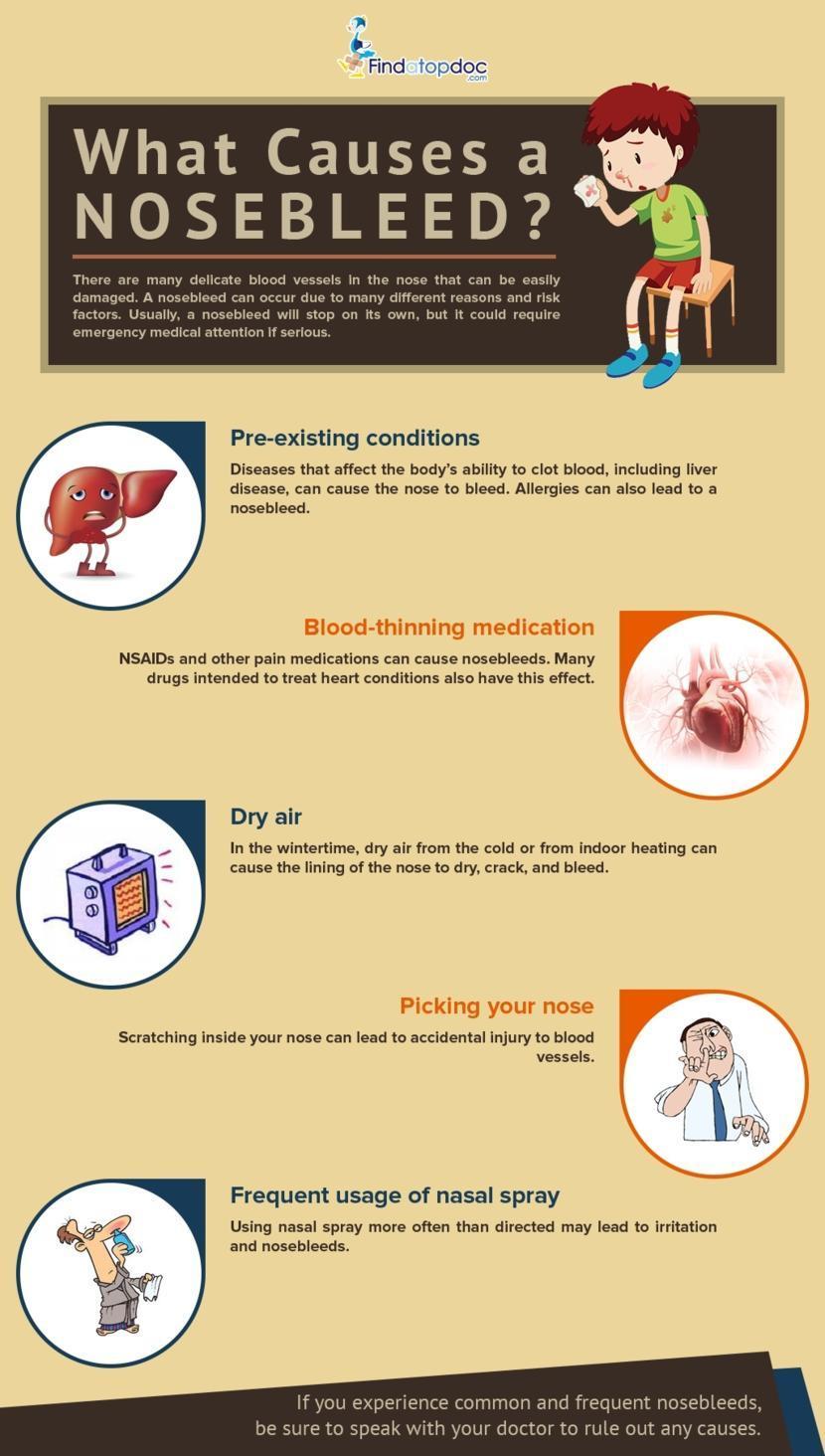
Nosebleed is common in winter, dry and cold season. There are two types of nosebleeds depending on the origin of bleeding – anterior nosebleed and posterior nosebleed.
Anterior nosebleed – this is the most common form of a nose bleed and comprises more than 90% of the symptom. As the name indicates, bleeding originates from the front part of the nose. It can be easily alleviated when compared to posterior nosebleed.
Posterior nosebleed – this is a rare form of nosebleed and is more commonly seen among elderly people. In this form, bleeding originates from a blood vessel at the back of the nose. This type of nosebleed is more complicated and may require medical attention for resolving the symptom.
Nosebleed is medically known as epistaxis. Nose has a rich network of blood vessels, any of which can bleed. Bleeding may occur from one or both the nostrils. The bleeding may last for few seconds or persist for more than 10 minutes. Bleeding may be light or heavy, depending on the cause.
Most forms of nosebleeds are not serious and resolve on its own.
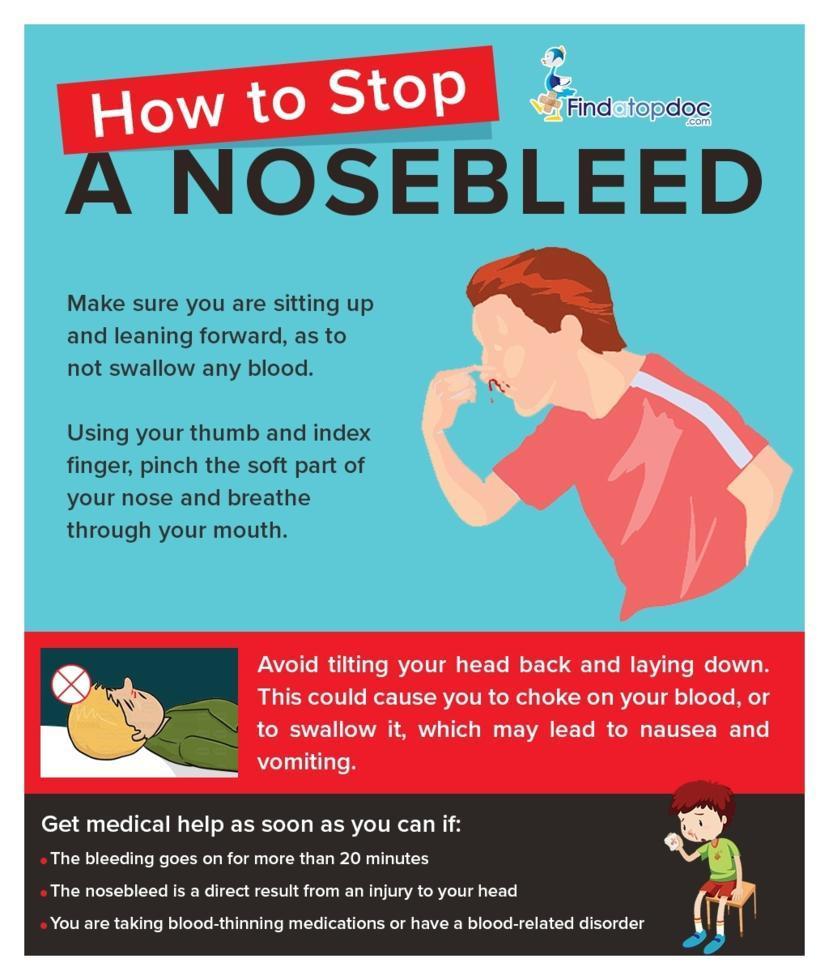
Further treatment or medical attention is needed if:
- One is taking blood-thinning medication
- The patient has blood-clotting disorder
- Associated symptom include anemia or breathlessness
- The child is under 2 years
- Nose bleeds are frequent
It is important to attend a hospital if bleeding continues for more than 20 minutes, or if bleeding is heavy. If the person swallows blood and vomit, it is important to get the person medical attention immediately.
Blowing nose hard enough to cause bleeding, picking nose, minor nose injuries, and changes in humidity and temperature are some of the common causes of a nose bleed.
It may also be caused by foreign objects stuck in the nasal cavity, chemical irritants, allergic reaction, upper respiratory tract infection, and taking large doses of aspirin. High blood pressure, clotting disorder, cancer, and bleeding disorder also have nose bleed as one of the symptoms.
The cause may be determined by physical examination and review of other symptoms. The presence of foreign objects in the nasal passages is checked during the examination. Information on current medications may also help in identifying the possible cause of the symptom.
There is no single, specific test to find the cause of a nosebleed. Tests like complete blood count, nasal endoscopy, clotting time, CT scan and X-ray may also be suggested to diagnose the cause of bleeding from the nose.
Simple home treatments may help to relieve bleeding. Squeezing the soft part of the nose while in sitting position often helps to stop bleeding. The nostrils should be closed for a short duration, during which breathing is done through the mouth.
Using a cold compress over the nose also helps to control bleeding. Decongestant nasal sprays may help to close the blood vessels. Frequent nose bleeds are treated by cauterization. Nose bleeds can be prevented by using a humidifier, avoiding picking nose, and limiting the use of aspirin.
Review of medical history and associated symptoms, in addition to physical examination, are very important in the diagnosis of the cause of a nosebleed. During the physical examination, the doctor may try to locate the origin of bleeding.
This will also help to find whether the bleeding is anterior or posterior. Other sources of bleeding will be diagnosed based on the person’s medical history and the findings of physical examination.
To make nasal examination less painful, the doctor may place a medication inside the nasal cavity using cotton. This medication helps to numb the inner part of the nasal cavity and constrict the blood vessels. This enables easy viewing of the small nasal cavity.
Nasal speculum is used to visualize the inside of the nose. The first step in diagnosis is the identification of the cause of anterior nose bleed. Diagnosis of the cause of posterior nose bleed is based on other tests and investigations that help in identification of the probable cause of bleeding.
Tests recommended in the confirmatory diagnosis include:
Complete blood count helps to check for blood disorders, while nasal endoscopy enables visualizing the interiors of nasal passages. Partial thromboplastin time is a test used to check the clotting time of blood. This is indicative of the presence of blood clotting disorders. X-ray or face and nose also may be used to determine the cause of the symptom.
Simple measures were taken up a home help in controlling bleeding. Squeezing or pinching the soft parts of the nose while in sitting position helps to stop bleeding. To prevent draining of blood into the throat, one should lean forward.
Sitting upright keeps the head at a higher position than the heart, reducing the pressure of blood flow. Applying an ice pack on the septum is another method to soothe the area.
Some of the common treatment methods used to treat nosebleeds include:
- Nasal packing – stuffing nasal sponges into the nose and pushing it back to apply pressure on the source of bleeding. This helps to prevent bleeding.
- Cauterization – cauterization is the burning and sealing off of the area from where bleeding originates. This is recommended if the blood vessel from which bleeding starts is identified.
- Septal surgery – this procedure is used to correct the deviation in the nasal septum. Repair of deviated septum helps in reducing the occurrence of nosebleeds.
- Ligation – tying the ends of the blood vessels that bleeds are known as ligation. In some cases, the artery that causes bleeding is also ligated. If the blood vessel is at the back of the nose, major surgery is recommended.
Most of the nosebleeds can be prevented:
- Using a humidifier at home during the dry day helps to reduce nose bleeds.
- Avoid picking nose to avoid trauma to the inner lining of the nasal cavities.
- Reduce intake of aspirin, the blood-thinning medication, that cause nose bleeds. This should be done only after discussion with the doctor.
- Limit the use of antihistamines and decongestants, both of which dry the nasal cavities.
Medical history and physical examination are the primary diagnostic procedures for identifying the cause of pustules. The doctor may ask questions about the onset of pustules or rashes, the regions where pustules started erupting, other associated symptoms, and trigger for pustules if any.
Other tests and investigations may be based on suspected cause of the condition. Complete blood count is used to check the levels of different blood cells. Erythrocyte sedimentation rate reveals the presence of inflammation.
Serum chemistry may reveal an increase in plasma globulins, albumins, calcium, and zinc. A culture of a sample from a pustule may be used to identify the causative organism.
Small pustules may resolve on its own without any specific treatments. Persisting small pustules can be alleviated by washing with warm water and a mild cleanser. This helps to remove the buildup of oil that leads to the formation of acne.
Many over-the-counter soaps and cream are available to remove small pustules. Topical products containing peroxide, salicylic acid, and Sulphur are also useful in treating pustules. Most of the topical products absorb the excess oil and dry the top layer of skin.
One must be careful as some products may make the skin excessively dry, leading to peeling off. Specialized products are available for sensitive skin. Pustules should not be squeezed or pinched as it may worsen the infection.
Moreover, it leads to skin damage in the region. Oil-based lotions and creams are not good for acne and pustules and should be avoided. These products aid in further buildup of oil in the pores, worsening the pustules.
Most of the pustules resolve with home remedies and conventional treatment methods. More aggressive treatment may be needed for those which do not respond to the usual treatment methods.
Persistent pustules are drained and stronger medications are recommended for relieving the symptom. For pustules caused by bacterial infections, prescription medications are suggested.
Oral antibiotics like amoxicillin and doxycycline are used to treat pustules caused by bacterial infections. Topical antibiotics like dapsone also may be useful. The dose of salicylic acid is increased to prescription-strength in these cases.
Photodynamic therapy is used for treating severe cases of pustules. This procedure involves the use of light and a special light-activated solution that helps to destroy a pustule.
This procedure is advantageous in that in addition to the pustules it also removes scars of old acne. It is known to make skin smoother. Other treatment methods depend on the underlying cause of the condition.
For example, corticosteroids, vit D3-derivatives, coal tar, anthralin, and retinoids are suggested for pustules caused by psoriasis. Topical and oral antibiotics are recommended for controlling rosacea as well.
Lindane, permethrin, Sulphur, hydrocortisone cream are suggested for the treatment of pustules caused by scabies. For viral infections, symptomatic treatment, adequate rest, and fluids are suggested. The pustules resolve when the infection reduces.
When left untreated, pustules may lead to severe complications, particularly if it is caused by infections. Abscess formation, encephalitis, endocarditis, meningitis, osteomyelitis, permanent scarring, pneumonia, sepsis, severe swelling, and tissue damage are some of the possible complications of pustules.