Important Things to Know about Disc Replacement Surgery
Dr. Harshpal Singh is a board-certified neurosurgeon who has advanced subspecialized training in both neuro-radiology and complex and minimally invasive spinal surgery. He has extensive experience treating a broad range of complex patient conditions using the latest treatment approaches. Dr. Singh attended medical school... more
Managing pain is one of the biggest challenges patients face when replacing an artificial disc. Like conventional orthopedic implants, lumbar disc replacement is a surgery that requires staying in the hospital for a few days and a series of conservative procedures at home over approximately three months. Therefore, what happens after lumbar fibrous cartilage replacement is vital for the rehabilitation of patients.
In addition, like all anesthesia-related surgeries, there are some risks associated with artificial disc replacement, such as trauma, nerve damage, infection, and sensitivity to the fake disc materials or shape.
What Is Disc Replacement Surgery?
Disc replacement surgery is one of the operations performed on the spine. The spine consists of bones called vertebrae. The intervertebral fibrocartilages act as protective shock absorbers that allow the vertebrae to rotate and move without the bones rubbing against each other. The discs and lumbar vertebrae are located at the end of the spine.
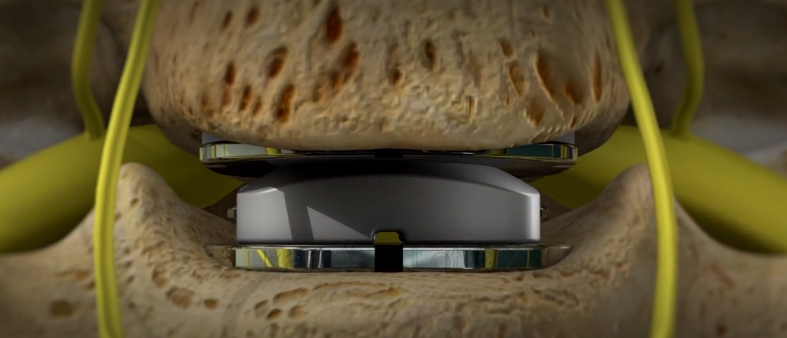
Spinal replacement surgery involves replacing the worn-out fibrous cartilage at the bottom of the spine with an artificial disc. The artificial disc is made of metal or a combination of metal and plastic. Disc replacement is usually seen as an alternative to the more common spinal fusion or drying surgery. Spinal replacement surgery requires general anesthesia and hospitalization.
An artificial disc, also known as a fibrocartilage prosthesis or spinal arthroplasty device, is a device that is inserted into the spine to provide functions similar to normal fibrocartilage functions associated with weight and movement.
The various forms of artificial fibrocartilage surgery are divided into two general categories: total disc replacement and disc core replacement. As part of the total disc replacement follow-up, as the name suggests, all or most of the fibrocartilage tissue is removed, and artificial fibrocartilage is placed in the intervertebral region. Only the middle of the disc (core or nucleus) is removed, which is replaced by an implant. The outer part of the disc (ring) is not removed.
Indications and Contraindications for a Disc Replacement
Indications for disc replacement may vary for each type of implant. Some common indications are pain from fibrocartilage that cannot be adequately reduced with non-surgical care like drug treatment, injections, chiropractic, or therapy. Usually, an MRI shows fibrocartilage degeneration. A discography is done to check if the fibrocartilage is related to your pain. The surgeon can correlate the results of these tests with the results of your medical history and physical examination to help confirm the source of your pain.
Many issues with artificial disc replacement may become an obstacle to this surgery. These include spondylolisthesis, osteoporosis, fracture of the vertebral body, allergy to materials in the device, spinal tumor, spinal infection, and morbid obesity, significant facet joint changes, pregnancy, chronic steroid use, or autoimmune problems.
You are not recommended to get an artificial disc if you have had previous abdominal surgery or if the condition of the blood vessels in front of your spine would increase the risk of significant injury during this type of spinal surgery.
The alternatives to fibrocartilage replacement include fusion or non-operative care. As a rule, surgery is not considered for the pain associated with the disk unless the pain has been severe for a long time and affects a patient’s quality of life and abilities.
The Risks of Disc Replacement Surgery
Disc replacement, like any other surgery, has its risks. These are:
- Possible problems with replacing the artificial disc
- Infection of the artificial disc or adjacent area
- Displacement or detachment of the artificial disc
- Breakage or failure of the prosthesis
- Spinal stenosis due to ruptured vertebrae
- Dryness or stiffness of the spine
- Blood clots in the legs due to reduced activity
Life After a Disc Replacement
A patient stays in the hospital a few days after the surgery. Since the disc prosthesis does not require bone fusion, the recovery time is shorter than with other spinal surgeries. If necessary, the patient is given pain medication and asked to get up and walk the next day.
The patient is taught to move properly and perform exercises such as gentle upper-body rotation. Exercise keeps the spine flexible and speeds up the healing and rehabilitation process.
As the healing process progresses, the patient is encouraged to walk and do stretching exercises. However, performing intense and irritating movements or activities is forbidden for some time. The recovery period lasts from several weeks to several months.
Spinal replacement surgery usually relieves pain but does not eliminate it. To have a reasonable and realistic expectation of the result of the operation, be sure to consult with your doctor before the procedure; also, ask your doctor for advice on postoperative care and how to care for your wound.








